Clinical trials in pediatric neuro-oncology: what is missing and how we can improve
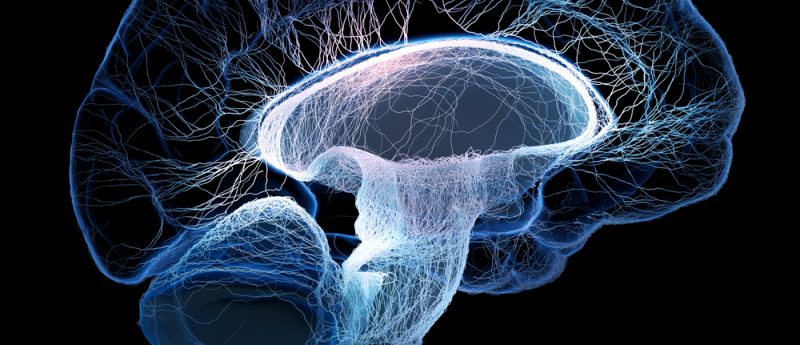
Brain tumors are the most common solid tumor in childhood, yet outcomes vary dramatically. High-grade gliomas have dismal outcomes with poor survival. By contrast, low-grade gliomas, have high survival rates, but children suffer from morbidity of tumor burden and therapy-associated side effects. In this article, we discuss how current trial designs often miss the opportunity to include end points beyond tumor response and thus fail to offer complete assessments of therapeutic approaches. Quality of life, neurocognitive function and neurofunctional deficits need to be considered when assessing overall success of a therapy. Herein, we identify specific end points that should be...