Use of cognitive tests to detect preclinical Alzheimer’s disease
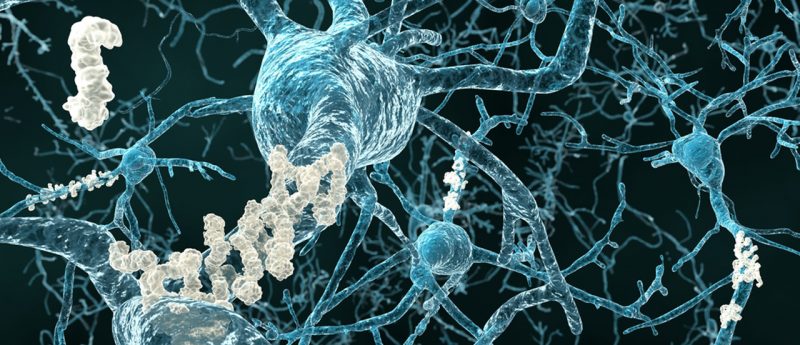
New research from the Keck School of Medicine of the University of Southern California (CA, USA) suggests that neuropsychological tests can detect early pre-clinical Alzheimer’s disease (AD) in older adults. The results from the meta-analysis, published in Neuropsychology Review, show that adults with amyloid plaques and tau pathology performed worse on cognitive tests. These novel findings could open up new avenues for early AD detection and management. Duke Han, Keck School of Medicine of the University of Southern California, explained: "In the last decade or so, there has been a lot of work on biomarkers for early AD. There are...