First signs of young-onset Parkinson’s detected in pluripotent stem cells
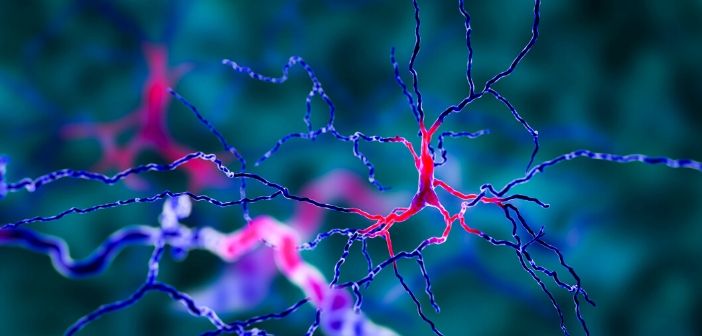
Research from Cedars-Sinai Medical Center (CA, USA) has demonstrated that cellular malfunctions associated with young-onset Parkinson’s disease could commence long before any outward symptoms. The study, published in Nature Medicine, also revealed that one particular drug could reverse the abnormalities in vitro. Parkinson’s disease occurs due to a loss of dopamine-producing neurons. In most cases, the cause of neuron failure is unknown, and there is currently no cure. In this study, researchers focused on investigating the mechanisms underlying young-onset Parkinson’s. "Young-onset Parkinson's is especially heartbreaking because it strikes people at the prime of life," commented Michele Tagliati (Cedars-Sinai), co-author of...