Sex-specific effects of microbiome perturbations in an Alzheimer’s mouse model: an interview with Hemraj Dodiya
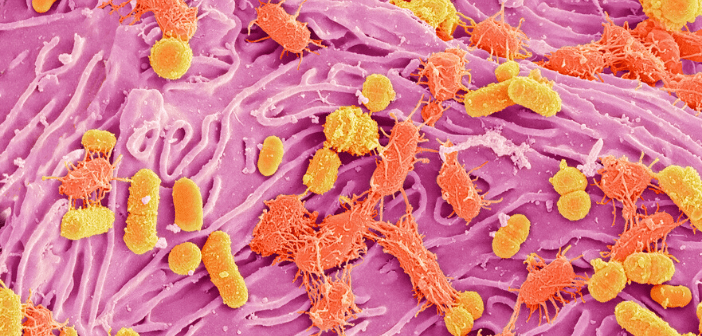
Hemraj Dodiya is a third-year postdoctoral scholar working with Professor Sangram Sisodia at the University of Chicago (IL, USA). He started his PhD in the field of Parkinson’s disease, where his dissertation focused on the microbiome gut–brain axis. Hemraj is currently utilizing his PhD as a basis to implement his expertise in this area to examine the microbiota gut–brain axis in Alzheimer’s disease. In this interview, Hemraj speaks to us about his work that was presented at SfN Neuroscience (19–23 October 2019, Chicago) on the sex-specific effects of microbiome perturbation on cerebral amyloid-β amyloidosis and microglia phenotypes in an Alzheimer’s...