SfN19: Metabolic disturbances in the brain may exacerbate and forewarn Alzheimer’s pathology in mice
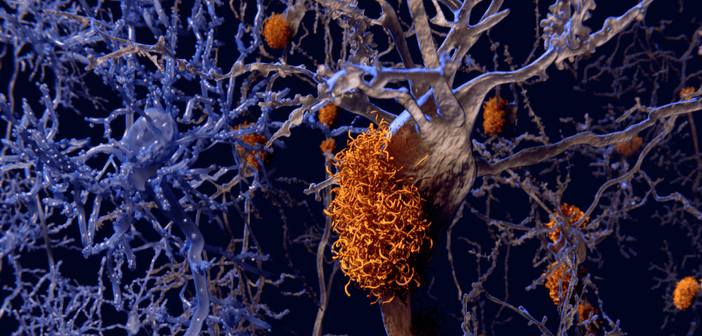
Recent research has implicated that Type 2 diabetes could increase the risk of Alzheimer’s disease (AD) by twofold. As metabolism of glucose is essential for brain functioning, including energy distribution and neural activity, any malfunction in this system would have cascading effects. Thus, researchers are working to understand the exact mechanisms that underpin the consequences of metabolic disturbances to more easily identify and treat diseases such as AD. At SfN Neuroscience 2019 (19–23 October, Chicago, IL, USA), three studies have been presented on the connection between dementia and the metabolic system that fuels the brain. David Holtzman (Washington University, MO,...