The future patient: what is pharma’s role?

‘Patient centricity’, ‘patient focus’ and ‘patient-centeredness’ are all terms that over the past decade have become everyday language in many areas of healthcare, not least in the pharmaceutical (pharma) industry, as players look to develop more relevant and appropriate products and services. Just in the 12.5 years since my own diagnosis with multiple sclerosis, I have witnessed an evolvement in the patient community and empowerment of the patient, as well as a definitive shift towards bringing the patient voice into the drug-development process. So, what is pharma’s role in the future patient landscape? How can and should the industry be partnering with patients?
What is it all about?
Personally, I don’t like the term ‘patient centricity’. It puts the patient at the center and other stakeholders on the outside, ‘feeding in’. This isn’t what the future is about for me. I much prefer the term ‘patient partnerships’ because healthcare is a complex journey involving multiple stakeholders that need to work together to achieve the best outcomes that put patient needs at the center.
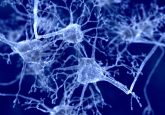
The patient community is becoming increasingly empowered and playing a bigger role in their healthcare decisions [1], not just in neurology but across many disease areas. The rise of the internet and so-called ‘democratization of information’ has meant that patients are more able than ever before to make key decisions about treatment plans and care pathways. As such, pharma is increasingly having to consider the patient earlier in the medicines development process, not just as an end user of products but as a key partner in their development. Additionally, pharma is also having to acknowledge that not all patients are a single homogenous group. The industry is now able to engage with different types of patients in different activities, based on their experience, skills, expertise and breadth of knowledge.
Why should pharma be partnering with patients?
Working with patients makes pharma’s work more relevant to the end customer, regardless of whether it’s gathering insights, a disease-awareness campaign or developing a clinical trial protocol. In many other industries it’s normal to consult end users when designing a product or service. Why should this be any different in drug development? Particularly in the area of clinical trials, a more patient-relevant research question and more patient-friendly design can improve recruitment and retention rates [2], which in turn can improve timelines and cost–effectiveness.
Partnering with patients can also foster greater innovation in a company, enabling an organization to serve unmet patient needs and increase competitiveness. Being able to demonstrate added value and patient involvement is becoming ever more important in the health technology assessment, as demonstrated by EMA and US FDA initiatives to ensure the patient voice is being heard [3,4].
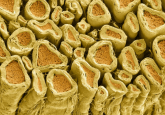
Patient partnerships can also improve employee motivation in pharma companies. It’s a constant reminder that there are people behind the disease. Patient partnerships can make employees’ work ‘come alive’, especially for those used to working with samples and data or purely dealing with clinicians and regulators. Motivated employees are generally more loyal and productive, plus a patient-focused ethos can help to attract the best talent.
Improving pharma’s reputation among patient communities is a mountain we are yet to conquer. “Pharma will never find a cure because it’s not profitable for them”, “they’re only making money out of us” and “they only see dollar signs, not humans” are all sentiments that frequently appear in discussions among patients. By taking practical steps to meet patient needs and by demonstrating a willingness to listen to and act on patient insights, pharma can start to rebuild trust, especially in communities that have long-standing mistrust of medical research [5]. Partnering with patient key opinion leaders and patient influencers plays a crucial role, as they are trusted members of the patient community.
Finally, patients also benefit from partnering with industry. They learn more about the drug-development process, can improve understanding of their own disease and can feel like they are helping their patient community. It is well documented that an informed patient often makes different decisions about their health [6], so any partnership that can support them in becoming more informed has to be a good thing. It will enable patients to make better decisions, foster change and create a more activated patient community.
Threading the patient voice throughout the medicines lifecycle
Whilst pharma has become quite good at engaging with patients in certain areas, there is still room for earlier involvement. Determining what is important to patients and using that to guide drug development is key for ‘getting things right’ from the very beginning. We can identify four broad areas within the research and development process where patients can be, and should be, involved: setting research priorities; research, design and planning; research, conduct and operations; and dissemination, communication and post-approval [7]. Within each area there is a multitude of different ways that pharma can partner with patients to make drug development more relevant and targeted to the intended community.
It’s not hard to find inspiration – a good starting place would be the many patient-centered conferences that are being held across the world that offer companies a platform to share examples of their work. Reuters Events’ ‘Pharma and Patient’ conference (formerly Eyeforpharma’s Patient Summit) and The Conference Forum’s ‘Patients as Partners’ are just two such conferences, bringing together patients, industry and patient groups to learn from each other. What is needed, however, is better guidance for pharma to form patient partnerships in a more meaningful way so that these relationships are longer lasting.
How can pharma form long-term relationships with patients?
In my experience there are five main principles for good patient partnerships: relevance, appropriateness, value, fairness and transparency.
A partnership needs to be relevant, not just a tick in the box. It means patients should be involved in the right projects at the right times during its lifecycle. Examples include designing clinical trials, disease awareness and education activities, patient support program development, events and meetings (both internal and external), development of patient-facing content and information (anything that will be read by, seen by or listened to by a patient should have patients involved in their development), and even involving patients in more strategic activities such as guiding a company’s patient-involvement strategy. From the outset, companies need to pinpoint every stage of a project timeline where patients could become partners.
Partnerships need to be appropriate and this involves acknowledging a patients’ particular experience, expertise and skills. In a disease-awareness campaign, for example, it would be most appropriate to partner with expert and professional patients to guide the campaign development and execution, but patients by experience would be most appropriate for telling their story within the campaign. Also, training and learning opportunities might be needed. Even the most experienced patient advocates will not know everything about every part of the medicines lifecycle – most of us ‘learn on the job’. Training, if required, should be seen as an investment, as it will facilitate more meaningful and effective engagement now and in the future.
Patient involvement should be valued. Different countries have different regulations regarding compensating patients for their time. If patients can be compensated, they always should be, and it should be appropriate to the task they’re involved in, their experience and their expertise. The National Health Council in the USA has developed a fair market value calculator that can be used as guidance [8]. It is being adapted for use in Europe too. If compensation isn’t allowed, a thank you, vouchers or donation to a patient association show that someone’s participation has been valued. A patient should never feel like they’re being ‘used’ or taken for granted within a partnership.
Fair partnerships mean taking into account someone’s circumstances and making patient collaboration accessible to all, not the domain of a select few. Patients are trying to manage their illness and live their lives, often under difficult circumstances. This means having realistic expectations and adapting working methods to make it easier for patients to partner with pharma. This might mean adjusting project timelines, arranging overnight accommodation for in-person events, making virtual options available where possible, reimbursing expenses in shorter timescales or paying them upfront, and/or making it easy for a caregiver to accompany someone. Considering these things not only makes the partnership fairer but also helps to ensure diversity of representation because it makes opportunities more accessible.
Finally, transparency is key to good pharma–patient partnerships. Setting out objectives and timelines, keeping patients informed of progress and feeding back on the value of their input are all important areas so that patients are certain of what their involvement looks like. Standard operating procedures should be explained, and legal documents should be clear and concise, utilizing plain language summaries as companion guides where necessary. Patients should never be left confused, unsure or frustrated by legal and compliance processes.
The future for pharma–patient partnerships
Moving patient partnerships beyond being a ‘nice thing to have’ to being a ‘business-as-usual’ process embedded within medicines development is definitely on the way. Changes in the industry, particularly over the last decade, have been encouraging, with companies and patient communities alike being much more open to collaborating in an effective way. What we need to ensure is that this role for pharma in empowering patients and making medicines development more targeted and relevant continues to be placed front and center of the industry moving forward.
[1] Neuro Central. Taking control and becoming empowered: the MS expert patient.
www.neuro-central.com/taking-control-and-becoming-empowered-the-ms-expert-patient/
[Accessed 25 November 2020]
[2] National Institute for Health Research. The balancing act: how patient engagement can improve recruitment and retention.
www.nihr.ac.uk/blog/the-balancing-act-how-patient-engagement-can-improve-recruitment-and-retention/20150
[Accessed 25 November 2020]
[3] European Medicines Agency. Training and resources for patients and consumers.
www.ema.europa.eu/en/partners-networks/patients-consumers/training-resources-patients-consumers
[Accessed 25 November 2020]
[4] US Food and Drug Administration. FDA patient engagement overview.
www.fda.gov/patients/learn-about-fda-patient-engagement/fda-patient-engagement-overview
[Accessed 25 November 2020]
[5] Hughes TB, Varma VR, Pettigrew C, Albert MS. African Americans and clinical research: evidence concerning barriers and facilitators to participation and recruitment recommendations. The Gerontologist 57(2), 348–358 (2015).
[6] NHS. Enabling people to make informed health decisions.
www.england.nhs.uk/ourwork/patient-participation/health-decisions/
[Accessed 25 November 2020]
[7] Geissler J, Ryll B, Leto di Priolo S, Uhlenhopp M. Improving patient involvement in medicines research and development: a practical roadmap. Ther. Innov. Reg. Sci. 51(5), 612–619 (2017).
[8] National Health Council. National Health Council patient engagement fair-market value calculator.
https://nationalhealthcouncil.org/fair-market-value-calculator/
[Accessed 25 November 2020]
Disclaimer
The opinions expressed in this editorial are those of the author and do not necessarily reflect the views of Neuro Central or Future Science Group.
You might also like: