Delayed onset paraparesis complicating epidural steroid injection with underlying spinal dural arteriovenous fistula
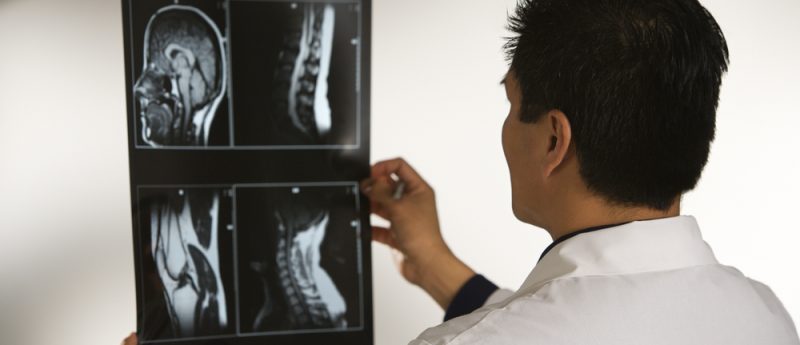
We report a case of a 48-year-old man with chronic back pain attributed to discogenic lumbar radiculopathy who underwent a fluoroscopy-guided L2–3 interlaminar epidural steroid injection. 4 h later, he developed acute paraparesis, sensory loss below T10 level and urinary retention. MRI of the thoracic spine revealed diffuse abnormal T2/FLAIR signal and extensive vascular flow voids. A spinal dural arteriovenous fistula was confirmed on spinal angiography. Embolization of the spinal dural arteriovenous fistula resulted in significant improvement of symptoms. We review previously reported cases and current understanding of the pathophysiology of this complication. All cases had symptom onset several hours...