Multiple sclerosis: potential risk factors, cognitive impairment and the microbiome
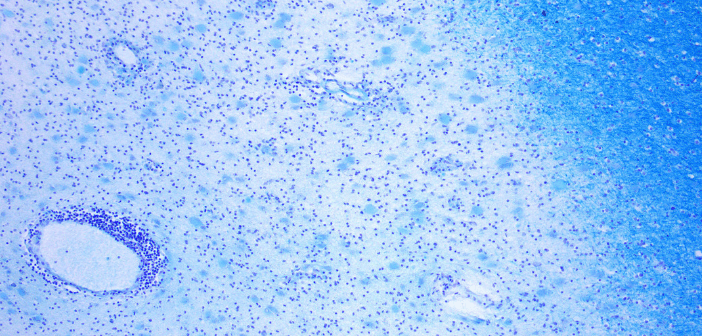
Marianna Cortese (MD, PhD) is a postdoctoral fellow at the Harvard School of Public Health (MA, USA) and is working in the research group of Dr Alberto Ascherio and Dr Kassandra Munger (both Harvard University). Marianna is currently focusing on multiple sclerosis (MS), including new potential risk factors of MS and cognitive impairment. In this interview, Marianna speaks to us about her talk on vitamin D, smoking, Epstein–Barr virus (EBV) and long-term cognitive performance in clinically isolated syndrome (CIS) patients: an 11-year follow-up study of the BENEFIT trial. She also discusses how the microbiome might play a role in disease...