SfN18: New strategies for identifying causes of vascular dementia
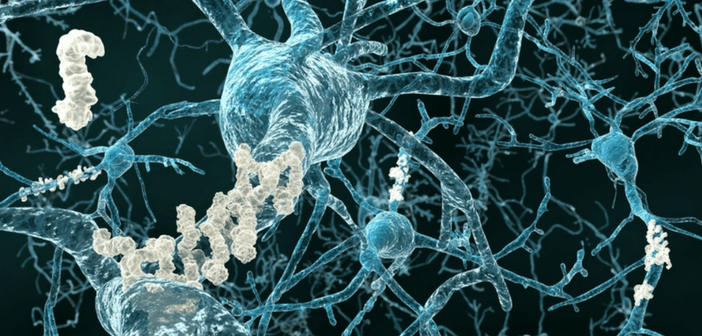
Studies that link breakdowns in the brain’s blood vessels to Alzheimer’s disease (AD) and vascular dementia were presented at SfN Neuroscience (3–7 November 2018, San Diego, CA, USA). Researchers anticipate that molecules that signal damage in these systems could aid in earlier detection of these diseases and inform more effective interventions. The research presented at the conference reveals new mechanisms for how damage to the brain’s vascular system contributes to neurodegeneration and point towards potentially protective or therapeutic interventions, such as exercise. Biomarkers for brain vascular injury could help identify dementia in its early stages In the first study presented,...