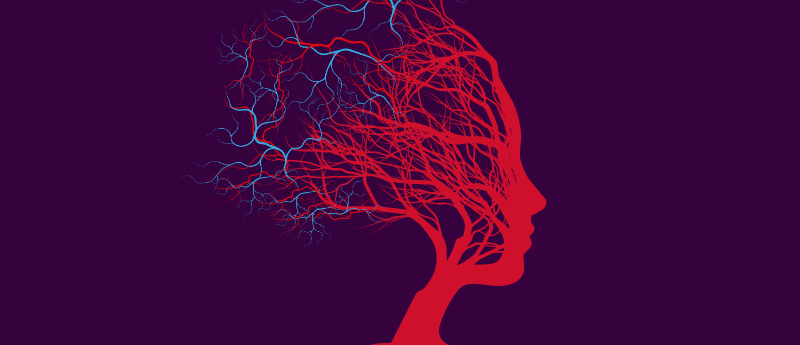
What role does the brain’s vascular system play in neurodegeneration?
 In this interview, we speak with Fanny Elahi (The Mount Sinai Hospital, NY, USA) about the captivating intersection of neuroscience and vascular biology. Elahi also shares her motivation for neuroscience, the pivotal role mentorship has played in her career and next steps in her research.
In this interview, we speak with Fanny Elahi (The Mount Sinai Hospital, NY, USA) about the captivating intersection of neuroscience and vascular biology. Elahi also shares her motivation for neuroscience, the pivotal role mentorship has played in her career and next steps in her research.
What motivated you to pursue a career in neuroscience and how have you overcome challenges along the way?
I have always been fascinated with the brain (from the PhD phase of my training) but clinical training focused my intentions. I was profoundly touched by patient stories and wanted to advance knowledge towards the development of treatments for brain degeneration caused by disease of the brain’s small blood vessels. My research became very clearly disease-focused. It is an exciting time to be working on brain degenerative diseases, because we are, for the first time, equipped with tools to tackle old questions and get closer to actionable answers. We have entered into the era of therapeutic developments for dementia-causing diseases!
I overcome challenges through grit, support and interactions within a fantastic community, which includes patients. To work on disease-oriented research one needs to deeply care about patients whose lives are most affected by the disease being studied. Creativity and talent do not suffice. It’s a marathon. To sustain our efforts and push past hard problems we need a constant source of motivation. For me, this motivation comes from seeing patients. We can’t stop until we have treatments and solutions.
How important has mentorship been in your career?
Mentorship is critical. The support of my mentors in large part is why I think of my years of training as some of the happiest years of my life. They are not easy – you don’t know if you’re going to make it and you work around the clock despite this very real sense of uncertainty. It says a lot about my mentors that I recall those years with such fondness. I may even miss them! I was learning every day. The ratio of impactful work to admin/bureaucracy was very different. I tell my trainees to enjoy this special time when you get to grow with protection. I take mentorship very seriously and aspire to provide the kind of mentorship to my trainees that I was fortunate to get from my mentors.
Any notable role models or organisations who influenced your journey?
Dr Bruce Miller (University of California, San Francisco, CA, USA) is a legendary mentor. A titan in dementia research, he is one of the most creative, wise, and kind human beings I have had the privilege to learn from and be mentored by. He mentors by example. He taught me that patients are at the center of discovery science and that they tell us where to look if we listen. No matter how busy he is, Bruce makes time for the clinic.
Are there specific policies or initiatives that you believe could enhance the work of women in neuroscience?
Data shows that women make outstanding leaders. I would like to see more women in leadership positions in neuroscience. More awards going to women is another side of the coin. These changes will be good for all and show women trainees that they can succeed with hard work and support.
What role does the brain’s vascular system play in neurodegeneration?
I would say a central role – this is at the heart of my lab’s research, so consider this to be the disclosure of my scientific bias. But I think the past few years have provided good data to suggest that we are on the right track! Vasculature is at the juncture of the brain and body, constantly exposed to blood (our environment), they filter what gets into the brain. As we age this process loses the needed selectivity and tightly organized microstructures, and we think this is an important component of brain aging and the risk for dementia. We are working on understanding the molecular code in order to develop treatments to protect the vascular barrier and connected microstructures of the brain. We think that sustaining healthy brain vasculature could slow down brain aging and push off dementia.
How could retinal scans be used to predict Alzheimer’s disease risk?
The eye and brain share biology. We have investigated the eye’s vasculature and have shown that vascular changes in the eye capture components of brain vascular aging. Much work remains to be done to see whether eye images can be used efficiently and whether they reflect sufficient components of the brain’s biology to be truly useful in the therapeutic discovery pipeline for brain degenerative diseases.
What are the key advantages of using a retinal imaging technique?
The main advantage is that it is non-invasive, fast and inexpensive. Patients already have to undergo so many tests and procedures; anything that allows us to assess them more comfortably and less invasively is a huge advantage. For instance, if we can find good connections to pathology that tracks with disease and responds to therapy, we could use the eye for monitoring response in clinical trials. This would be huge.
Interviewee profile:
Fanny Elahi is a physician-scientist and Associate Professor of Neurology, Neuroscience, and Pathology, Molecular and Cell-Based Medicine. Elahi completed medical school and a doctorate in neurogenetics, residency in neurology and fellowship in neurodegenerative disorders to gain multi-disciplinary domain knowledge, clinical, scientific and technical skills required to build a therapeutically-oriented translational research program in neurodegenerative diseases.
Guided by a commitment to patient care, the Elahi Lab leverages clinical insights to design laboratory research to uncover molecular links between disease of the brain’s vascular system with neurodegeneration. They aim to treat dementia by understanding the role of blood vessels in human brain function and the genetic causes of vascular pathology across the lifespan that may cause a spectrum of dementia-related diseases. The Elahi Lab’s multidisciplinary approach combines deep clinical, cellular and molecular phenotyping to model disease, identify early biomarkers and find therapeutic targets for vascular brain dysfunction and degeneration. The team focus on human tissue and biospecimen for discovery of molecular dysregulations and modeling mechanisms in iPSC-derived multi-cellular in vitro models. Much of the work underway is centered on early detection of neurodegenerative disease and discovery of treatments for genetic risk factors, such as CADASIL, an autosomal dominant disease that causes vascular cognitive impairment (VCI) and APOE4, the most prevalent risk allele for Alzheimer’s disease. If you are interested in participating or contributing to this research, please reach out us: www.elahilab.com
The opinions expressed in this article are those of the author and do not necessarily reflect the views of Neuro Central or Taylor & Francis Group.