A peek behind the paper – Fabrício Figueiró on the characterization and antiproliferative activity of glioma-derived extracellular vesicles
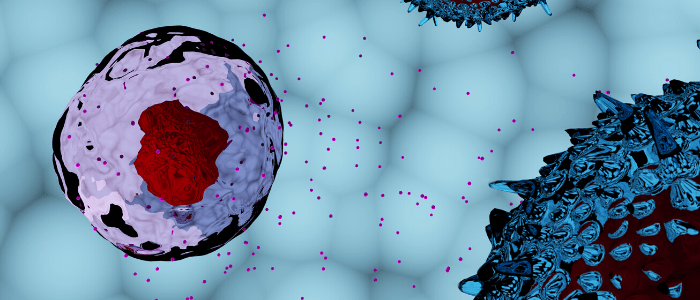
In this 'peek behind the paper' series, we take a look behind the scenes of a recent Research Article from Nanomedicine entitled, 'Characterization and antiproliferative activity of glioma-derived extracellular vesicles', where we ask corresponding author, Fabrício Figueiró (Universidade Federal do Rio Grande do Sul, Brazil), about his study into characterizing a method to isolate glioma-derived extracellular vesicles (GEVs) and understanding their role in immune system modulation and glioma progression. Please can you introduce yourself and explain what stimulated your interest in using immunology and nanomedicine to treat gliomas? My name is Fabrício Figueiró, I’m a pharmacist with a PhD and...