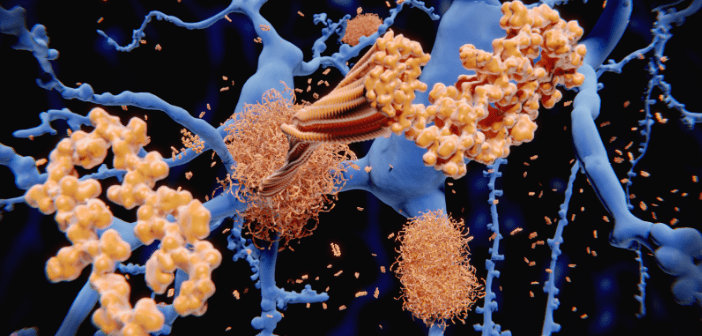
AAT-AD/PD™ 2020: an insight into the first fully virtual Alzheimer’s and Parkinson’s disease conference
Back in September 2019, I submitted my abstract to present a poster at the AAT-AD/PD™ Focus Meeting in Vienna (Austria). This was to be my first international conference and I was excited for the chance to talk to leaders in the field around the world about my research. By the time March came around, it seemed more and more likely that the conference would never happen thanks to the COVID-19 outbreak. However, the message from AAT-AD/PD™ was consistently that they would do everything they could to avoid cancelling the conference. To their word, 3 weeks before the conference was due...