Inflammatory disease and anxiety: could endocannabinoids be a mechanism of comorbidity?
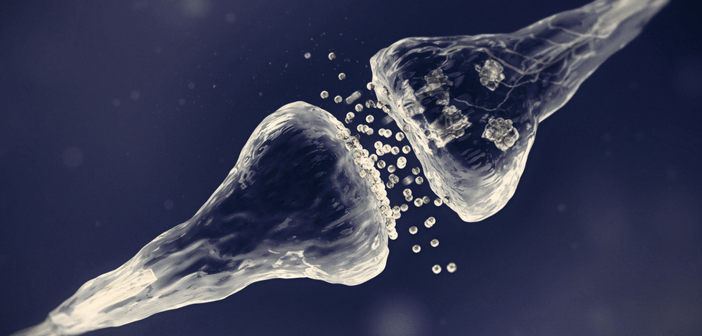
Matthew Hill is an Associate Professor at the Hotchkiss Brain Institute at the University of Calgary (Canada). His research primarily focuses on trying to understand the endocannabinoid system and how it regulates emotions and stress circuits in the brain to modulate anxiety and stress-related psychiatric disorders, such as post-traumatic stress disorder. In this interview, Matthew speaks to us about his talk on endocannabinoids as a mechanism of comorbidity between inflammatory disease and anxiety, including what the next steps of his research will be. He also discusses if the controversial elements behind term ‘cannabinoid’ provide any limitations to research. You’re presenting...