iPSC therapy success in Parkinson’s monkey models
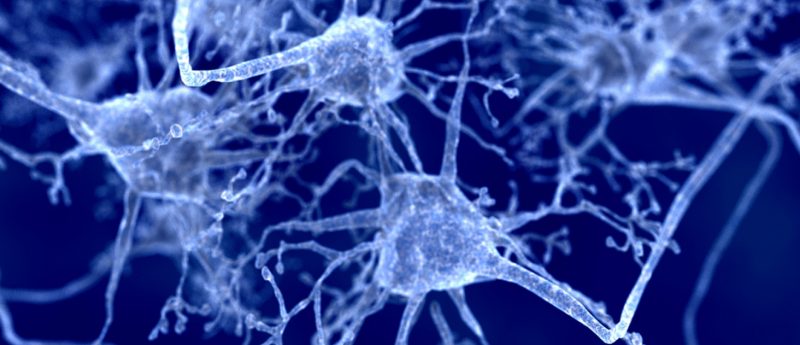
Researchers from Kyoto University (Japan) have shown that human induced pluripotent stem (iPS) cell-derived dopaminergic (DA) progenitor cells can survive and function as midbrain dopaminergic neurons in a primate model of Parkinson’s disease (PD). The first study of its kind, this new research marks a major breakthrough in bringing iPS cell-based therapies for neurodegenerative disease closer to the clinic. Previous clinical trials have explored the use of fetal-derived stem cells for PD, though the use of these cells remains controversial. This new preclinical study, however, published this week in Nature, has been hailed as being the final step before the...