Neuroinflammation and Alzheimer’s disease: the role of microglia in brain homeostasis
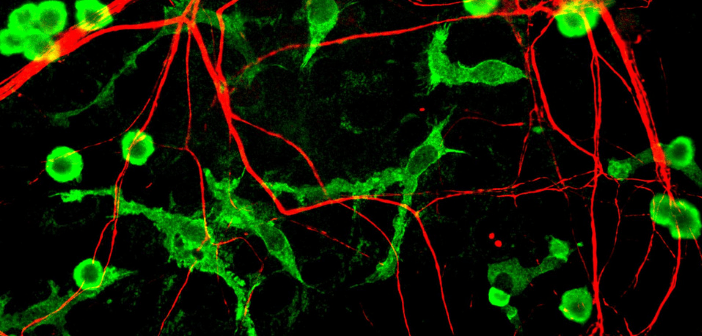
Credit: Gerry Shaw/Wikimedia Commons​​​
Hugh Perry is a consultant at the Dementia Research Institute at University College London (UK) and leads the Neuroinflammation Theme across the Dementia Research Institute Centers. His job is to encourage and foster collaboration in neuroinflammation across the Institutes and to use its intellectual capital and fantastic resources to gain insights into neurodegeneration disease process. Previously, Hugh trained as a neuroscientist at the University of Oxford (UK), he then moved to the University of Southampton (UK) to continue to lead a laboratory in neuroinflammation. In this interview, Hugh speaks to us about a big topic in dementia research right now,...