Could Alzheimer’s variability be explained by different brain atrophy patterns?
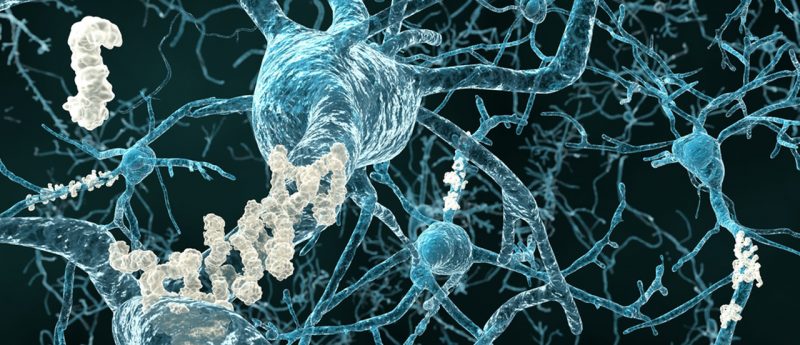
Researchers at Massachusetts General Hospital (MA, USA) and the National University of Singapore (Singapore) have demonstrated that variation in the symptoms of Alzheimer’s disease (AD) could be explained by differences in brain atrophy patterns. Utilizing mathematical modeling, the team identified specific atrophy patterns that appear to be related to the loss of particular cognitive abilities, indicating that different atrophy patterns may explain how AD can manifest in individual patients. "The symptom severity and neurodegeneration can vary widely across patients in AD," explained Thomas Yeo (Maschusetts General Hospital). "Our work shows that participants in this study exhibit at least three atrophy...